
Background: Long-term survivors of childhood Hodgkin lymphoma (HL) are at significant risk for cardiovascular, pulmonary, and endocrine morbidity in addition to subsequent cancers. Emerging evidence suggests that HL survivors may also experience persistent neurocognitive impairment, however the prevalence of neurocognitive impairment has not been well characterized. Further, little work has been done to examine how specific treatments or comorbidities are associated with these impairments.
Methods: The current study included 1,760 survivors (52.0% female, mean[sd] 37.5 [6.0] years old, 23.6 [4.7] years from diagnosis) of childhood Hodgkin lymphoma and 3,180 sibling controls (54.5% female, 33.2 [8.5] years old) from the Childhood Cancer Survivor Study. Participants completed questionnaires assessing four domains of neurocognitive impairment (task efficiency, emotional regulation, organization, and memory). Impairment for each domain was defined as a score worse than the 90th percentile of community controls. Treatment exposures were abstracted from the medical record. Second malignancies (SMN) were self-reported and subsequently confirmed by pathology findings or medical record review. Chronic health conditions were self-reported and systematically graded according to the NCI CTCAE v4.3 (Grade 1 mild, Grade 2 moderate, Grade 3 severe/disabling, Grade 4 life-threatening). Generalized estimating equations were used to calculate risk of impairment in survivors compared with siblings adjusted for age, sex, and race. Among HL survivors, multivariable log-binomial regression was used to calculate risk of impairment associated with demographic, clinical, and treatment factors. Separate models examined risk associated with Grade 2+ chronic health conditions adjusted for age, sex, and race.
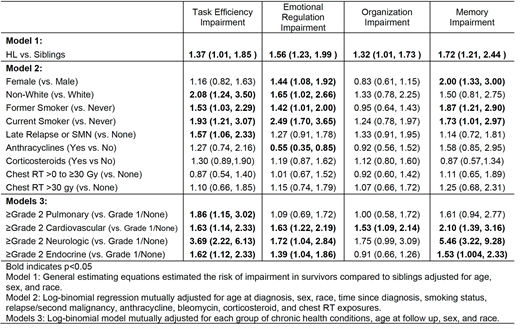
Results: 10.8% of HL survivors reported impaired task efficiency (vs. 7.7% in siblings), 16.6% emotional regulation (vs. 11.5% in siblings), 12.1% organization (vs. 10.3% in siblings), and 8.1% memory (vs. 5.7% in siblings). Compared with siblings, survivors reported significantly higher risk of impairment in each of the four neurocognitive domains after adjusting for age, sex, and race (Table).
Female survivors had elevated risk of impairment on emotional regulation (RR [95%CI] 1.4 [1.1,1.9)) and memory (2.0 [1.3,3.0]). Compared with white survivors (91.8% of the population), non-white survivors had higher risk of impairment in task efficiency (2.1 [1.2, 3.5]) and emotional regulation (1.7 [1.0,2.7]). Current smokers (12.3%) had higher risk of impairment in task efficiency (1.9 [1.2, 3.1]), emotional regulation (2.5 [1.7,3.7]), and memory (1.7 [1.0,3.0]).
Having a late-relapse (>5 years from diagnosis) or a second malignancy (20.0%) was associated with elevated risk of impairment in task efficiency (1.6 [1.06,2.3]). While not statistically significant, anthracycline exposure (39.8%) was associated with higher risk of impairment in task efficiency (1.3 [0.7,2.2]) and memory (1.6 [0.9,3.0]). No statistically significant associations were noted for bleomycin, corticosteroids, or chest radiation.
HL survivors with pulmonary morbidity (8.5%) had a higher risk of impairment on task efficiency (1.9 [1.2,3.0]) compared to those without. Cardiovascular conditions (32.9%) were associated with elevated risk of impairment in all domains (RR range from 1.5 to 2.1, all p<0.05, Table). Endocrine (54.3%) and neurologic conditions (6.6%) were associated with an increased risk of task efficiency, emotional regulation, and memory impairments (RR range from 1.4 to 5.5, all p<0.05, Table).
Conclusions: Survivors experienced significantly more neurocognitive impairment compared to sibling controls. Among survivors, potentially modifiable risk factors such as smoking and chronic health conditions were associated with neurocognitive impairment while treatment exposures showed little association. Mitigation or prevention of smoking and chronic health conditions may improve neurocognitive functioning in HL survivors
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal